Yamada, Thoru, and Elizabeth Meng. Practical Guide for Clinical Neurophysiologic Testing: EEG. Available from: Wolters Kluwer, (2nd Edition). Wolters Kluwer Health, 2017.
Greenfield, John, L. et al. Reading EEGs: A Practical Approach. Available from: Wolters Kluwer, (2nd Edition). Wolters Kluwer Health, 2020.
Capecchi F, di Giacopo A, Keller E, Mothershill I, Imbach LL. Stimulus Induced Rhythmic, Periodic, or Ictal Discharges (SIRPIDs) and its Association with Non-convulsive Status Epilepticus in Critically Ill Patients. Clinical EEG and Neuroscience.
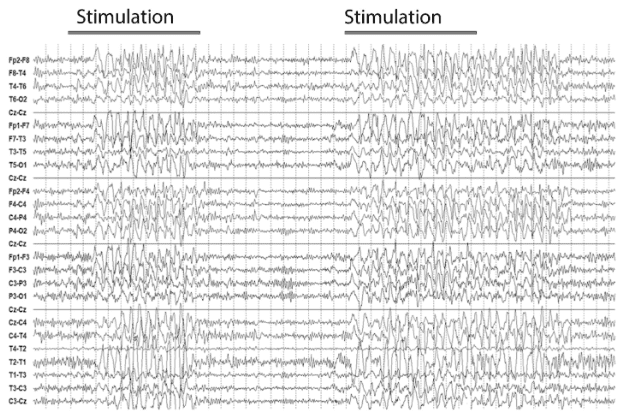
Stimulus-induced (or stimulus-exacerbated) rhythmic, periodic, or ictal discharges (SIRPIDs) are felt to represent the stimulation of thalamocortical circuits by hyperexcitable or damaged cortex. These discharges occur with state changes, spontaneous self-arousal, or external stimulus such as auditory or tactile in the critically ill patient population. SIRPIDs can resemble ictal discharges, usually lasting <10-15 seconds and terminating with the end of stimulation or spontaneously.
This umbrella term includes all SI- patterns together (SI-RDA, SI-PDs, SI-SW, SI-IIC, SI-BIRDs, or SI- seizures).
When documenting or reporting, the clinician should refer to the specific “SI–" pattern instead of the term “SIRPIDs,” and specify the type of stimulus induced (auditory; light tactile; patient care and other non-noxious stimulations; or noxious: suction, sternal rub, nailbed pressure, nostril tickle, trapezius squeeze, or other).
SIRPIDs may consist of variable waveforms, ranging from blunt sharp-wave triphasic form to spike-wave discharges. This often makes it difficult to decide if the patient should be treated as having a seizure.
Question:
In long term monitoring of critically ill patients, stimulations to assess background reactivity should be performed how often?
Results
#1. In long term monitoring of critically ill patients, stimulations to assess background reactivity should be performed how often?
Clinical and EEG reactivity should be assessed daily. The presence of any sedating medications and the timing of their administration should be recorded. Optimally, reactivity testing is performed after fixing any electrode problems. Because fixing electrodes is a type of stimulation, reactivity should be assessed from the time the patient is first stimulated. The stimulus used for reactivity testing should be recorded, and an institutional protocol for reactivity assessment may be useful. For certain indications, such as monitoring for ischemia, more frequent checks of reactivity are helpful and can be incorporated into nursing assessments and annotated on the EEG record.